Greater Occipital Neuralgia
Greater Occipital Neuralgia Review
Could This Be The Cause of Your Headaches?
Greater Occipital Neuralgia (ON) Diagnosis and Presentation
The greater occipital nerve (ON) has been recently considered one of few uncommon causes of intractable headaches. The term occipital neuralgia refers to neuropathic pain experienced in areas supplied by occipital nerve and presents similarly to migraines. Most commonly, occipital neuralgia presents unilaterally with radiation to the frontal, orbital and periorbital regions, and tenderness on palpation over the suboccipital region.
The tenderness experienced may prevent patients from brushing their hair, wearing a hat, or lying on a pillow. The pain occurs along the superior path of the greater ON, following its exit from the semispinalis capitis or the trapezius muscle.
Similarly to migraines, patients with ON can present with trigger points over the neck and shoulder. ON is most often idiopathic, but can occur as result of whiplash injuries, compression of the upper cervical roots by arthritic changes in the spine (rheumatoid arthritis), or compression of the nerve between the atlas and axis.
Pathomechanics of The Greater Occipital Nerve
ON can involve the greater (GON), lesser, or least occipital nerves. The GON comes from the medial branch of the dorsal ramus of C2. The GON travels between the inferior oblique capitis muscle and semispinalis capitis and pierces the semispinalis. The GON provides cutaneous sensory innervation to the posterior scalp from the external occipital protuberance to the vertex.
The proposed mechanism of irritation is due to anatomical entrapment and irritation due to myofascial spasm along the nerve’s path. Some sites of entrapment include where the GON branches from C2 between the axis and the atlas, between the inferior oblique (deeply) and semispinalis (superficially), and as it pierces the belly of the trapezius.
The entrapment site at the C2 branch can be exacerbated during rotation as the inferior facet of the atlas compresses the nerve against the superior facet of the axis.
The entrapment site between the inferior oblique and semispinalis can be aggravated during flexion-extension as the nerve is stretched over the inferior oblique which acts as a pivot point.
The GON can be either aggravated as it wraps around the inferior oblique or as it pierces the semispinalis.
Alternatively, this entrapment site can be tested by compressing 2 cm lateral and 1 cm inferior to the spinous process of C2. The entrapment at the upper trapezius aponeurotic band (the nerve moves superiorly, laterally, and superficially as it emerges from the semispinalis) can be due to local inflammation or compression by the greater occipital artery. Spasm of the trapezius is unlikely a cause of compression as it will pull the aponeurotic band inferiorly and away from the GON, which would decompress the nerve.
Signs & Symptoms of Greater Occipital Nerve Headaches
The hallmark of GON is paroxysmal lancinating pain that is described as stabbing, shooting, electric, or shock-like pain from the occiput radiating to the vertex. If a dull occipital ache is the primary complaint, then it is more likely to be due to occipital referral pain and cervicogenic headache. A C2 neuralgia or post herpetic neuralgia of the C2 nerve root presents similarly with lancinating occipital pain and can result from compressive or inflammatory lesions. Temporal arteritis of the occipital artery should also be considered as a differential since it presents with scalp tenderness and occipital headache.
Who Can Diagnose GON?
This condition can be diagnosed by a physiotherapist or chiropractor near you without the need for a doctor’s referral. During your assessment the health care provider will be ruling in and out similar conditions including:
Cervical Radiculopathy or Cervical Disc Herniation
Cervicogenic Headache
Myofascial Pain Syndrome (Upper Trapezius, Sternocleidomastoid, Suboccipitals)
Whiplash Associated Disorder
The assessment is important for determining the root cause of your symptoms. As you can imagine, without an appropriate diagnosis the rehab programming can easily become mismanaged. Treating the wrong diagnosis is similar to fixing a flat tire by changing the car door - it won’t give you the result you are looking for as the root problem was not addressed. Get assessed today in-person or through virtual appointments by clicking the button below.
Treatments for GON
Treatments can be delivered by your local massage therapist, chiropractor, physiotherapist, or osteopathic manual practitioner. A complete treatment may include elements of:
Cervical Facet Joint Mobilization or Manipulation (Joint Oscillations or Adjustments)
Soft Tissue Therapy (Ischemic Compression, Myofascial Release, or Deep Tissue Massage)
Instrument Assisted Soft Tissue Mobilization (Graston, Scraping)
Cupping
Acupuncture / Electroacupuncture
Proprioceptive Neuromuscular Facilitation / Post Isometric Relaxation Muscle Energy Techniques
Rehab Exercises
You can book in an appointment with a Rehab Hero clinician by clicking the button below.
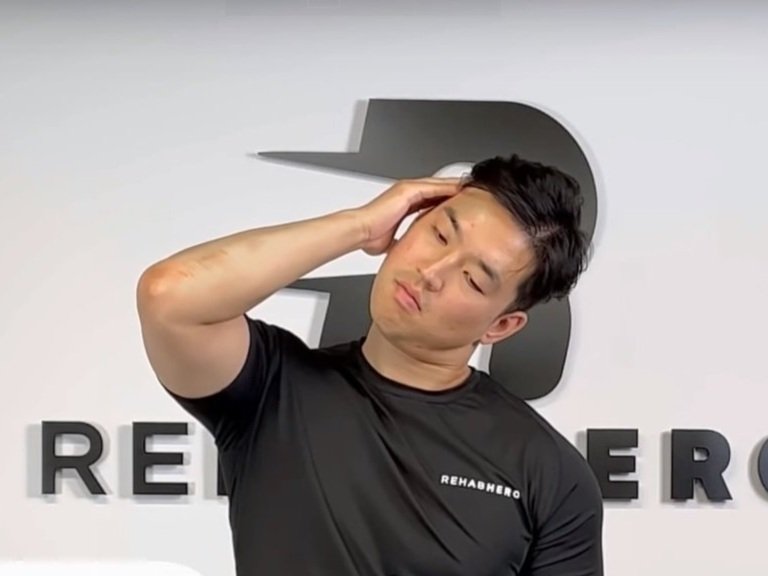
Which Rehab Exercises Can Help with Occipital Neuralgia?
At the beginning of a rehab program for this condition, one of the main goals is to de-load the amount of work that the muscles surrounding the nerve experiences. Some exercises that serve to complete this purpose include:
In addition to the above exercises it will also be important to address related issues such as Thoracic Hypomobility, Apical Chest Breathing, Stress Management, and Sleep Quality. To learn more about your specific issue you can book in an appointment with a qualified health care professional by clicking the button below.
Written By:
Dr. David Song, Chiropractor, Strength Coach
References
1. Dougherty C. Occipital neuralgia. Current Pain & Headache Reports [serial on the Internet]. (2014, May), [cited July 13, 2017]; 18(5): 411. Available from: CINAHL Plus with Full Text.
2. Loukas M, El-Sedfy A, Tubbs R, Louis R, Wartmann C, Jordan R, et al. Identification of greater occipital nerve landmarks for the treatment of occipital neuralgia. Folia Morphologica [serial on the Internet]. (2006, Nov), [cited July 13, 2017]; 65(4): 337-342. Available from: MEDLINE with Full Text.
3. Cesmebasi A, Muhleman M, Hulsberg P, Gielecki J, Matusz P, Loukas M, et al. Occipital neuralgia: anatomic considerations. Clinical Anatomy (New York, N.Y.) [serial on the Internet]. (2015, Jan), [cited July 13, 2017]; 28(1): 101-108. Available from: MEDLINE with Full Text.
4. Sahai-Srivastava S, Ling Z. Occipital Neuralgia With and Without Migraine: Difference in Pain Characteristics and Risk Factors. Headache: The Journal Of Head & Face Pain [serial on the Internet]. (2011, Jan), [cited July 13, 2017]; 51(1): 124-128. Available from: Nursing & Allied Health Collection: Comprehensive.