Thoracic Outlet Syndrome Review
Thoracic Outlet Syndrome
Anatomy and different types of thoracic outlet syndrome compression sites
What Is Thoracic Outlet Syndrome?
Thoracic Outlet Syndrome (TOS) is a group of disorders that involve the compression of 1 or more neurovascular bundle as they travel through the thoracic outlet (1). Current literature states that there are 5 types of TOS, namely arterial TOS (A-TOS), venous TOS (V-TOS), traumatic neurovascular TOS, true neurogenic TOS, and disputed TOS (1). Disputed TOS is the most poorly understood category of the 5, it is without any consistent clinical features due to any specific anatomical variation or abnormality, and no reliable method of testing (1). It is better understood as cervicoscapular pain syndrome which is beyond the scope of this learning objective.
Anatomy Of The Thoracic Outlet
The neurovascular bundle involved with TOS extends from the base of the neck to the axilla (armpit) and contains 3 regions. The first region is the interscalene triangle which is bordered by the anterior scalene, middle scalene, and first thoracic rib (FTR) (1). The second region is the costoclavicular space which is bordered by the FTR, clavicle, and the anterior scalene insertional point posteriorly (1). The third region is the subcoracoid space which lies just beneath the pectoralis minor tendon (1). The neurovascular bundle is comprised of the brachial plexus, and the subclavian and axillary arteries and veins (1). TOS is the compression of at least one of these elements.
Anatomy of the Brachial Plexus
The brachial plexus can be further divided into 3 clinically relevant smaller plexi. The supraclavicular plexus represents the C5-T1 nerve roots, and the upper, middle, and lower trunks. The retroclavicular plexus consists of the 3 anterior divisions and 3 posterior divisions. Finally, the infraclavicular plexus represents the lateral, posterior, and medial cords, musculocutaneous nerve, axillary nerve, median nerve, radial nerve, and ulnar terminal nerves (1). The supraclavicular plexus can be further subdivided into the upper plexus (upper trunk and C5-6 nerve roots), middle plexus (middle trunk and C7 nerve root), and lower plexus (lower trunk and C8-T1 nerve roots)(1).
Neurogenic Thoracic Outlet Syndrome
True neurogenic TOS (TN-TOS) is also known as classical TOS, and cervical rib and band syndrome (1). TN-TOS most often is presented in young to middle aged females with symptoms into the dominant hand (1). In this condition, the lower plexus (C8-T1) is stretched and angled superiorly, often due to either a hypertrophied anterior scalenes, a cervical rib, or by an inferiorly located fibrous band that extends from the FTR to the C7 rib or elongated transverse process (1).
Due to the inferior location of the T1 APR relative to the C8 APR, it tends to be stretched out more than C8 (1). This causes muscles innervated by T1 to be more affected than other involved muscles, namely the muscles of the thenar eminence (thumb) may experience weakness or muscle wasting. Associated findings may include impaired fine motor skills (1). Muscle weakness and atrophy will be most pronounced in the median nerve distribution (thenar muscles), followed by the ulnar nerve, and then the radial nerve. However, due to the slow natural history of TN-TOS, muscle fiber reinnervation is capable of keeping up with any denervation that may occur, and may not be well represented in the early stages of progression (1). Sensory changes are much more commonly affected than changes seen in muscle weakness or wasting. Paresthesias will most commonly follow the lower plexus distribution (C8, T1).
Arterial Thoracic Outlet Syndrome
Arterial TOS often involves unilateral compression of the subclavian artery and is considered a rare entity (2). Causes of A-TOS include a large bony anomaly, deformed first thoracic rib (FTR), anterior or middle scalenes hypertrophy, or intramuscular fibrous bands (2). Vessel compression may cause intimal damage, turbulent blood flow, thrombus formation, distal embolization, aneurysm, poststenotic dilation, and effort-related symptoms of claudication (2). Common signs and symptoms include chronic upper extremity ischemia, pain with effort, easy fatigability, claudication, extremity coolness, pallor, decreased capillary refill, audible bruit, and diminished or absence of distal pulses (2). In more severe cases, a painless pulsatile mass may be identified with subclavian artery aneurysm, distal ulcerations may be observed and are indicative of thrombus formation, and severe ischemia and tissue necrosis may be identified indicating the need for amputation (2). Advanced imaging is warranted if A-TOS is suspected.
Venous Thoracic Outlet Syndrome
V-TOS is also a rare form of TOS and is due to unilateral venous thrombus formation in the subclavian or axillary veins, and is associated with repetitive upper extremity activities (baseball or swimming) or underlying thrombotic disorder (2). This condition affects more men than women, usually affects the dominant limb, and may result in venous hypertension following activity (2). Acute occlusion manifests itself rapidly, with upper extremity swelling, palpable clotted axillary veins, cyanosis, and pain (2). Chronic thrombosis manifests itself as dilated veins in the neck, chest, and shoulder (2).
Disputed Thoracic Outlet Syndrome
Disputed TOS has a high prevalence, affects women more than men, and is often bilateral. Often this condition is lumped together with TN-TOS due to the impact it has on the brachial plexus despite different pathomechanics (2). This condition occurs with a compression or distraction injury of the brachial plexus. 4 mechanisms have been proposed, they are congenital anomaly, trauma (single acute or repetitive microtrauma), poor posture, or any combination of these (2). This condition may be presented with scalene muscle fibrosis, spasm of congenital musculotendinous ligaments, traction induced scarring of the brachial plexus, or muscle imbalances (2).
What Are The Signs & Symptoms?
Thoracic Outlet Syndrome pain patterns can vary depending on which part of the plexus is compressed. Clinically, sensory complaints are the main symptoms experienced by patients, either as pain or paresthesias for disputed TOS (2). An upper plexus and lower plexus pattern have been developed. In lower plexus pattern the pain is experienced in the neck and radiates down the medial arm, forearm and hand, with sensorimotor abnormalities following the C8/T1 pattern (2). Upper plexus pattern has pain in the shoulder which radiates into the ipsilateral head and neck, anterior-posterior aspect of the thorax, and proximal arm, with sensorimotor abnormalities following a C5/C6 distribution (2). Occipital or orbital headache, facial pain, facial numbness, anterior chest wall pain, and intrinsic hand muscle weakness may also be reported (2).
Due to the location of the affected nerves, thoracic outlet syndrome can not affect your legs.
How To Test for TOS?
Provocative tests including Adson’s, Wright’s, costoclavicular, and EAST maneuver may be positive. These can be completed by your physiotherapist or chiropractor. If you suspect that you may have one of the types of thoracic outlet syndrome, contact your healthcare provider to be diagnosed. In Ontario, no referral is needed by your medical physician for physiotherapy or chiropractic.
What Are My Treatment Options?
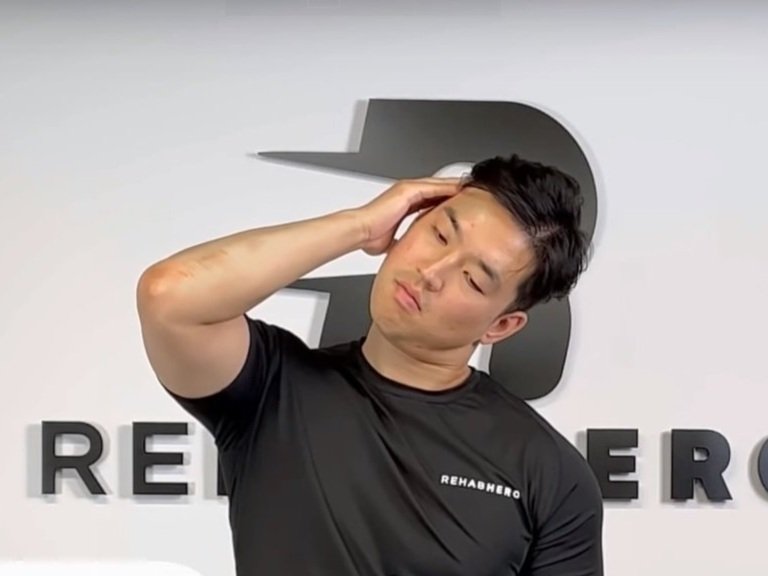
Depending on the severity of thoracic outlet syndrome surgery may be recommended by your healthcare provider. For less severe forms of TOS conservative forms of therapy may help with recovery. Both chiropractic and physiotherapy have shown to be helpful for the reduction of symptoms and pain using a combination of myofascial release therapy and exercise prescription. Massage therapy also may help as an additional type of intervention to alleviate symptoms by reducing muscle tension at compression sites for certain types of Thoracic Outlet Syndrome.
References
1. Ferrante M, Ferrante N. The thoracic outlet syndromes: Part 1. Overview of the thoracic outlet syndromes and review of true neurogenic thoracic outlet syndrome. Muscle & Nerve [serial on the Internet]. (2017, June), [cited November 8, 2017]; 55(6): 782-793. Available from: CINAHL Plus with Full Text.
2. Ferrante M, Ferrante N. The thoracic outlet syndromes: Part 2. The arterial, venous, neurovascular, and disputed thoracic outlet syndromes. Muscle & Nerve [serial on the Internet]. (2017, Oct), [cited November 8, 2017]; 56(4): 663-673. Available from: CINAHL Plus with Full Text.